Degenerative joint disease/Osteoarthritis
Degenerative joint disease/Osteoarthritis is a painful condition that results in the deterioration of the cartilage tissues that support the weight-bearingjointsin the body. It occurs when the cartilage that cushions the ends of bones in your joints gradually deteriorates.
Cartilage is a firm, slippery tissue that permits nearly frictionless joint motion causing pain and stiffness around thejoint.
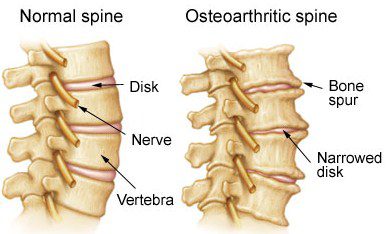
In osteoarthritis, the slick surface of the cartilage becomes rough. Eventually, if the cartilage wears down completely, you may be left with bone rubbing on bone.
When you move a joint, the joint expresses fluid from the pressure. When the pressure is relieved, the fluid diffuses back together with oxygen and nutrients. This is why the health of the cartilage depends on movement of the joint.
There are three common forms of osteoarthritis, and many people will have some of each type.
All people will develop it to some degree, involving one or more joints, throughout a lifetime because of aging. The most common sites for Osteoarthritis include the base of the thumb joint, the knees, and the hands.
The first and very mild form causes bone enlargement of the joints in the fingers. The second form involves the spine, where bony growths appear on. And the third form involves the weight-bearing joints, most often involving the knees, which are followed by the hips.
Osteoarthritis symptoms often develop slowly and worsen over time. Signs and symptoms of osteoarthritis include:
- Pain –Your joint may hurt during or after movement.
- Tenderness –Your joint may feel tender when you apply light pressure to it.
- Stiffness –Joint stiffness may be most noticeable when you wake up in the morning or after a period of inactivity.
- Loss of flexibility –You may not be able to move your joint through its full range of motion.
- Grating sensation –You may hear or feel a grating sensation when you use the joint.
- Bone spurs –These extra bits of bone, which feel like hard lumps, may form around the affected joint.
Factors that may increase your risk of osteoarthritis include:
- Older age –The risk of osteoarthritis increases with age.
- Sex –Women are more likely to develop osteoarthritis, though it isn’t clear why.
- Obesity –Carrying extra body weight contributes to osteoarthritis in several ways. The more you weigh, the greater your risk. Increased weight puts added stress on weight-bearing joints, such as your hips and knees. In addition, fat tissue produces proteins that may cause harmful inflammation in and around your joints.
- Joint injuries –Injuries, such as those that occur when playing sports or from an accident, may increase the risk of osteoarthritis. Even injuries that occurred many years ago and seemingly healed can increase your risk of osteoarthritis.
- Certain occupations –If your job includes tasks that place repetitive stress on a particular joint, that joint may eventually develop osteoarthritis.
- Genetics –Some people inherit a tendency to develop osteoarthritis.
- Bone deformities –Some people are born with malformed joints or defective cartilage, which can increase the risk of osteoarthritis.
Currently, the process underlying osteoarthritis cannot be reversed. However, symptoms can usually be effectively managed with lifestyle changes, physical and other therapies, medications, and surgery. Exercising and achieving a healthy weight are generally the most important ways to treat osteoarthritis.
You may want to consider procedures such as:
- Cortisone injections –Injections may relieve pain in your joint. During this procedure your doctor numbs the area around your joint, then places a needle into the space within your joint and injects medication. The number of cortisone injections you can receive each year is generally limited to three or four injections. This is because the medication can worsen joint damage over time.
- Lubrication injections –Injections of hyaluronic acid may reduce pain by providing some cushioning in your knee, though some research suggests these injections offer no more relief than a placebo. Hyaluronic acid is similar to a component normally found in your joint fluid.
- Realigning bones –If osteoarthritis has damaged one side of your knee more than the other, an osteotomy might be helpful. In a knee osteotomy, a surgeon cuts across the bone either above or below the knee, and then removes or adds a wedge of bone. This shifts your body weight away from the worn-out part of your knee.
- Traction:This technique involves the chiropractor holding one end of the degenerative joint and pulling the two bones/ends away from each other. This alleviates pressure off the nerves and therefore helps reduce the pain.
- Joint replacement.In joint replacement surgery (arthroplasty), your surgeon removes your damaged joint surfaces and replaces them with plastic and metal parts. Surgical risks include infections and blood clots. Artificial joints can wear out or come loose and may need to eventually be replaced.
Dr. Harmony Mir can detect the earliest degenerative changes in the joints. She can see the impact of degenerative changes in the spine, as well as the hips, knees, and other weight-bearing joints. She is also trained to relieve the pain and improve joint function throughchiropractic manipulation, trigger-point therapy, and soft tissue therapies such as massageandActive Release Technique. Dr. Mir can also help youchoose exercises that are best to reduce joint pain.